What is Unicondylar (Unicompartmental) Knee Replacement?
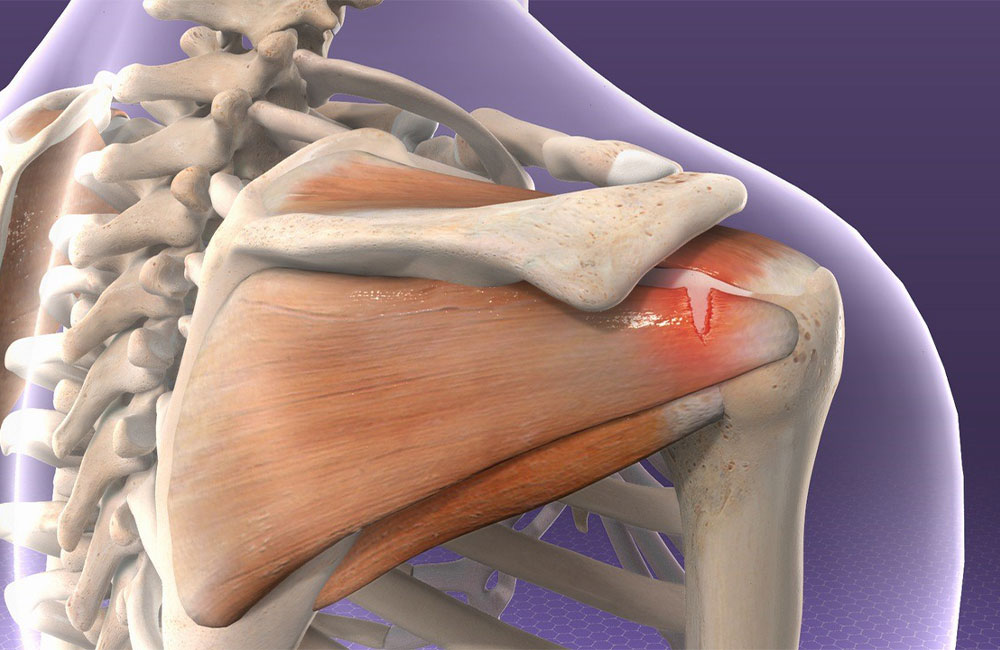
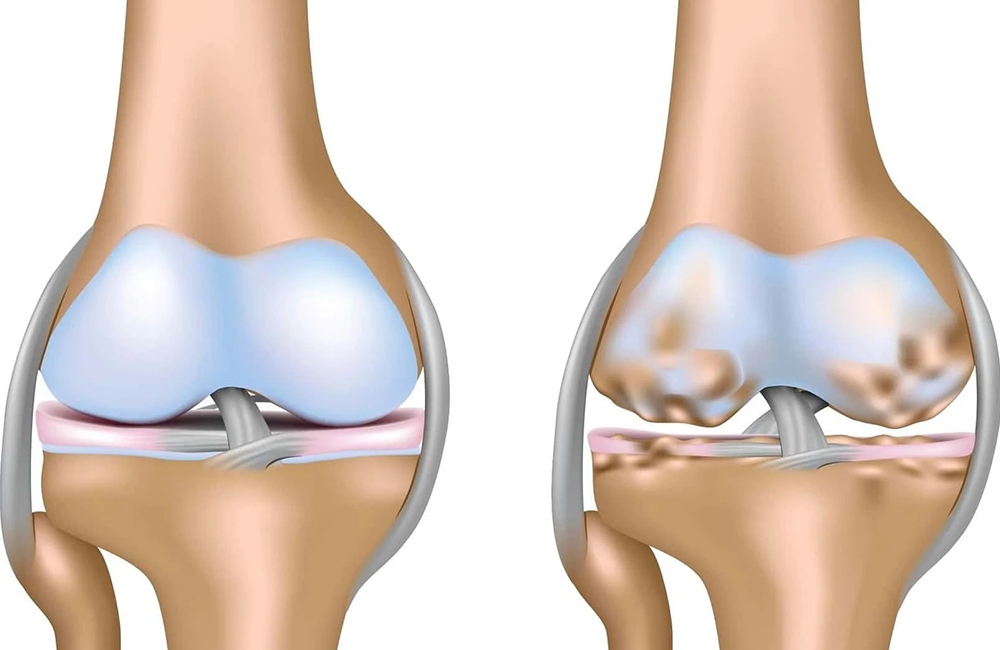
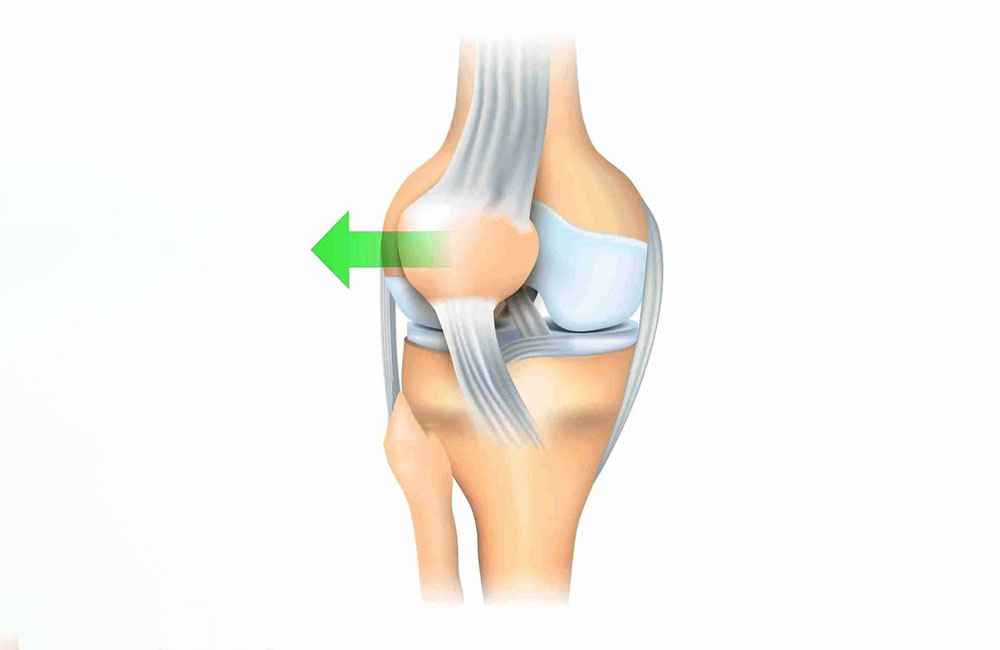
Unicondylar (Unicompartmental) Knee Replacement: Knee replacement surgeries generally yield very good results. However, the inability to fully restore the natural feeling of the knee may leave some patients dissatisfied. Therefore, various knee replacement options have emerged for different patients, with unicondylar knee replacement being a significant alternative. The knee joint consists of two condyles in the femur (thigh bone). These condyles can be thought of as two different wheels. In standard total knee replacement, both condyles and their corresponding surfaces are replaced with a metal prosthesis. However, damage in many patients is often limited to just the inner condyle and its corresponding surface. The unicondylar prosthesis only replaces the damaged condyle and its surface. Studies suggest that approximately half of patients who undergo total knee replacement could have been treated with a unicondylar prosthesis.
What are the Advantages of Unicondylar Prosthesis?
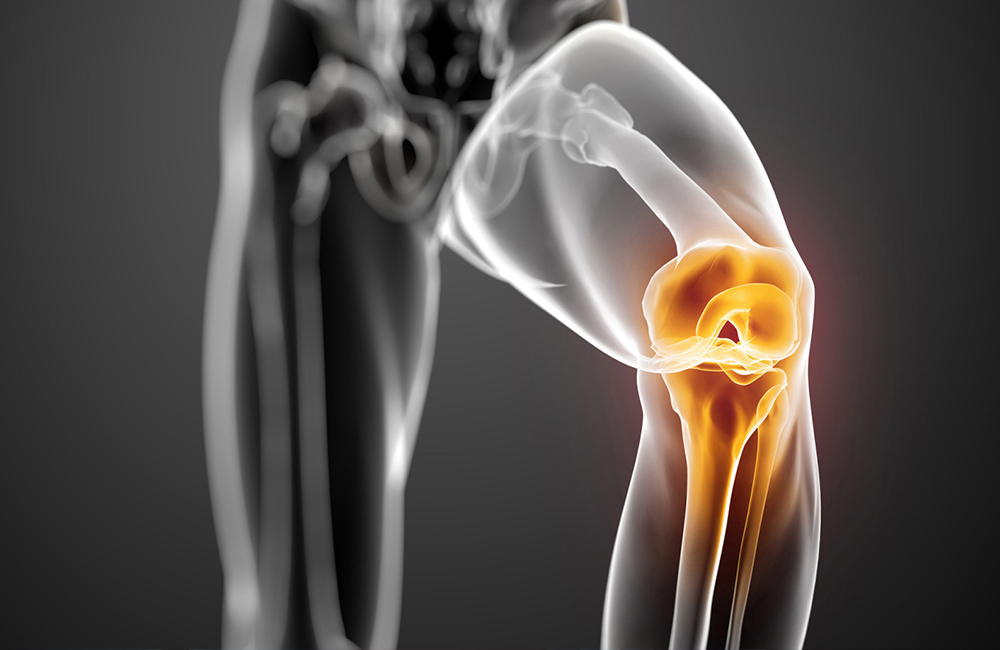
Unicondylar prostheses are generally performed through much smaller incisions (7-10 cm), minimizing damage to the muscles around the knee. Patients typically have shorter rehabilitation times and recover more quickly to their daily activities. With smaller incisions and less muscle cutting, the risk of infection and wound complications is also reduced.
Since only half of the knee is replaced, patients regain a more natural feeling and kinematics of the knee more quickly. Compared to total knee replacement, patients experience a much more natural walking motion.
Is Unicondylar Prosthesis Suitable for Every Patient?
There are specific criteria for patients who may receive a unicondylar prosthesis. The most important criterion is that the wear in the knee must be limited to a single compartment. Patients with damage in both compartments are not suitable candidates for this surgery. After taking X-rays of your knee, your doctor can provide information regarding your suitability. In ambiguous cases, MRI and CT scans may be requested.
Another criterion is the integrity of the anterior cruciate ligament (ACL). The proper functioning of the ACL is crucial for the natural kinematics of the unicondylar prosthesis. This can be evaluated during your examination, and in uncertain cases, an MRI may be necessary.
Other criteria include weight and age. In particular, patients with obesity (BMI over 35) are typically recommended to undergo total knee replacement rather than unicondylar. Age is a relative criterion, and the decision regarding a patient’s suitability is made in consultation with a doctor, considering the patient’s overall health.
Before Surgery
Before surgery, patients are examined, and their complaints are clearly defined. In many cases, plain X-rays are sufficient for diagnosis and treatment planning. Additionally, an MRI scan and leg length alignment X-rays may be requested. Once surgery is planned, any current medications, especially anticoagulants, will be adjusted accordingly. An anesthesiologist will evaluate you to determine the most suitable anesthesia method, which may be spinal anesthesia (numbing the lower body) or general anesthesia (being fully asleep). A fasting period of approximately 6-8 hours is required before surgery.
During Surgery
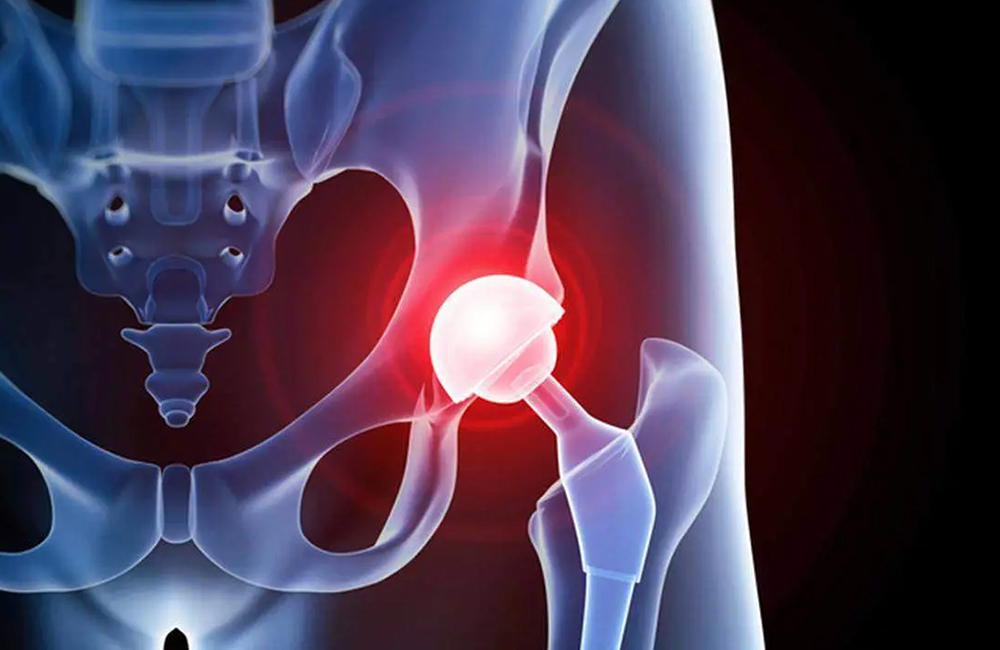
During the surgery, a 7-10 cm incision is made on the front of your knee to access the joint. Using special guides, the damaged cartilage and menisci are removed, and a suitable space is prepared for the new prosthesis. After trying out the options, the appropriate prosthesis is placed in the knee. To prevent blood accumulation in the knee, a drain tube is inserted and will be removed painlessly after 24 hours. You will then be taken to your room for post-operative care.
After Surgery
Patients are typically encouraged to get up and walk the day after surgery. On the first day, in-bed exercises for knee range of motion and strengthening the thigh muscles are initiated. Patients usually become ready to go home within 2-3 days.
For the first 15 days, a walker is often used, and afterward, a cane may be used for 2-4 weeks. Generally, by 4-6 weeks, patients can walk independently. Your doctor will provide exercises to perform at home during the first three months.
Patients usually regain the ability to perform daily activities at home after about 15 days, can typically drive within 3-4 weeks, and gradually return to their daily routines.
Surgery Outcomes
Patients can expect pain-free and unsupported walking in the long term after unicondylar knee replacement. The knee joint can fully flex and extend, allowing patients to perform daily activities like kneeling. This is a highly successful procedure with over 90% survival rates over a ten-year period.
Risks
As with any surgery, there are risks associated with unicondylar knee replacement, including infection and bleeding. To prevent infection, antibiotics will be given before and for 2-3 days after surgery. Medications will be adjusted to minimize bleeding risk, and patients may be asked to wear special stockings for about a month. There is also a risk of fractures in case of falls, and the implanted prosthesis may require replacement due to wear over time.
Q&A
Is unicondylar knee replacement a preliminary surgery before total knee replacement?
No. Unicondylar knee replacement is performed when wear is limited to a single compartment, allowing for prolonged use without the need for total knee replacement.
Can unicondylar prostheses be done at younger ages?
Yes, unicondylar prostheses are preferred for suitable patients in the younger age group (50-65).
Do you also perform unicondylar prostheses in older age groups?
Yes, if the patient’s overall health is appropriate and the knee damage is suitable for unicondylar replacement, it can be safely performed in older patients.
For detailed information, visit my YouTube channel: @profdrhalukcabuk