Total Hip Replacement Surgery is a treatment method applied to patients who experience pain in the front part of the hip and groin, leading to difficulties in daily activities.
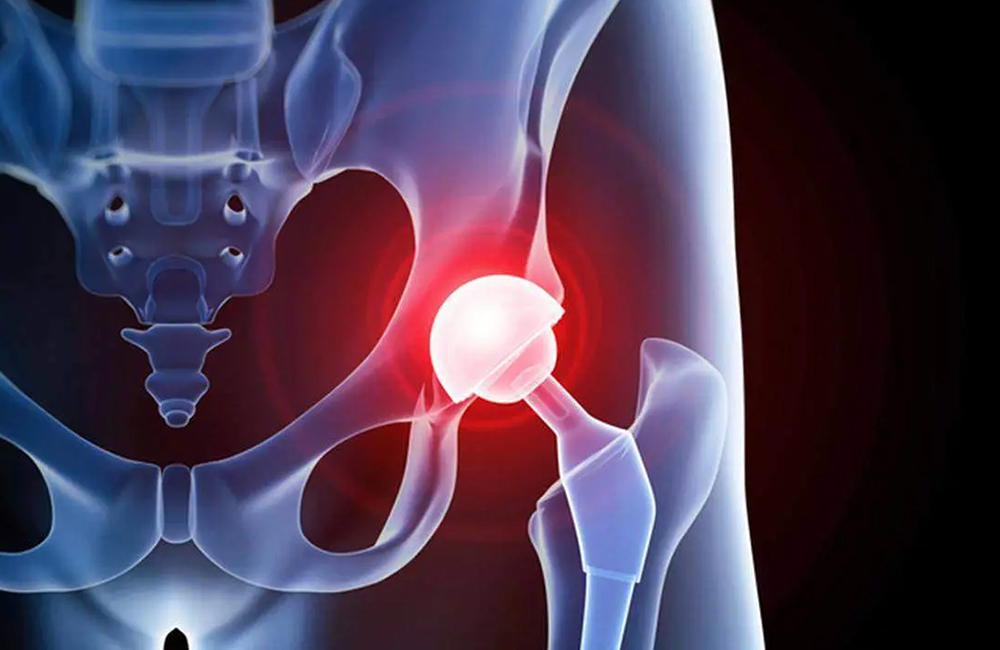
The hip joint is a ball-and-socket type joint with a wide range of motion. When there is damage to either the ball-shaped part (the upper part of the femur) or the socket (the part of the pelvis that forms the joint), the function of the joint is impaired, resulting in pain. In total hip replacement, both parts of the joint are replaced with an artificial joint.
When is Total Hip Replacement Indicated?
Your doctor may recommend total hip replacement surgery if you experience pain, limited mobility, and damage to your hip joint.
Total hip replacement is indicated in cases of:
- Persistent and recurrent pain unresponsive to pain relief medications
- Needing a cane or walker to walk
- Pain severe enough to wake you from sleep
- Difficulty getting up from a seated position
- Struggling with stairs
This procedure could be suitable for you.
Factors Leading to Hip Joint Damage
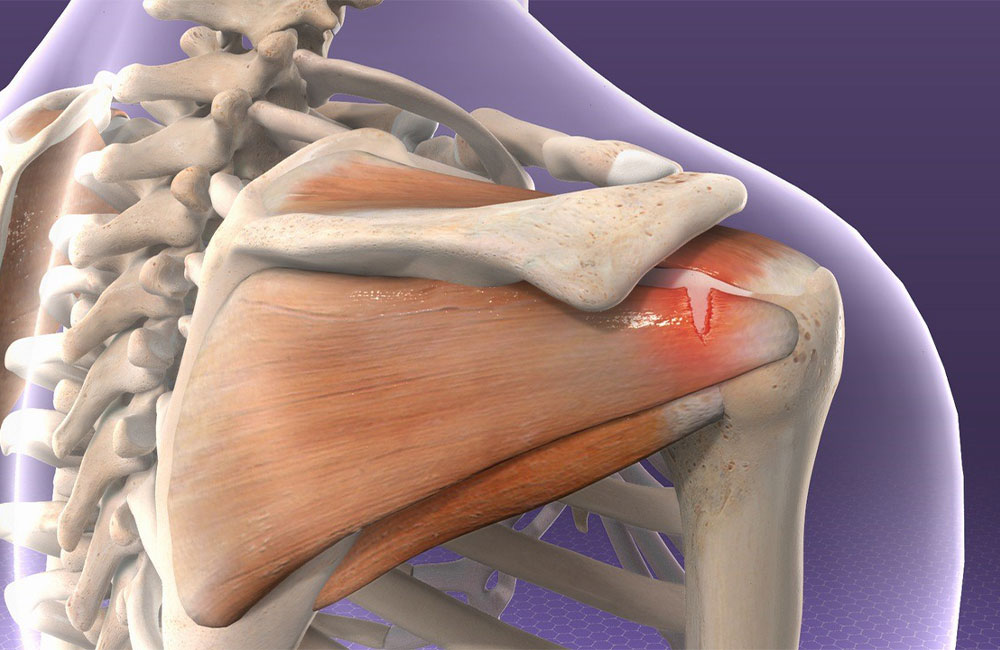
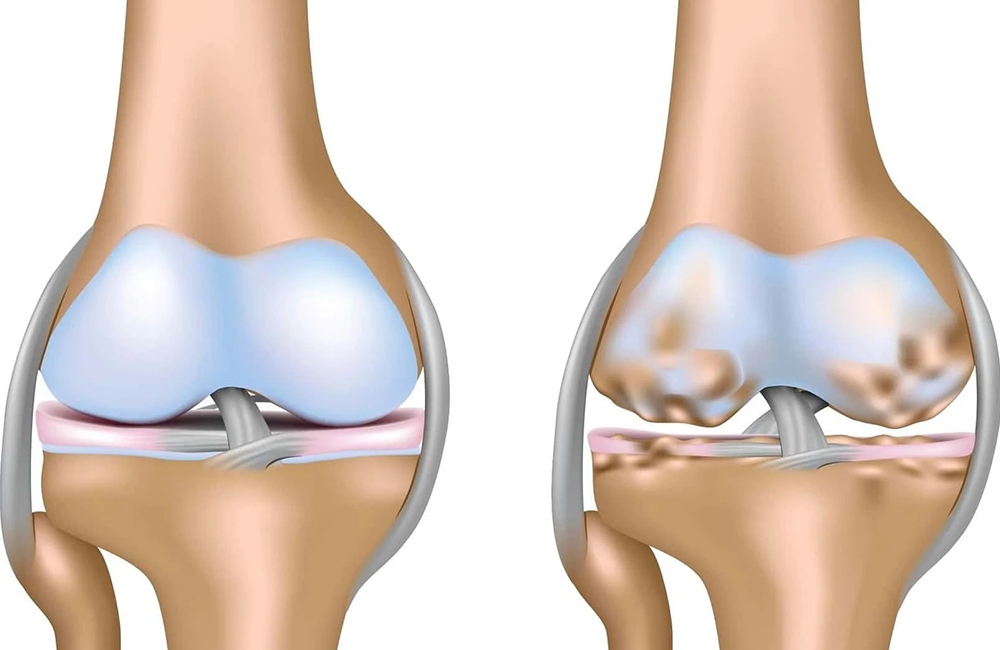
Osteoarthritis: Caused by the gradual wear and tear and damage to the cartilage in the hip joint.
Rheumatoid Arthritis: Rheumatic diseases can affect all joints, including the hip joint, leading to damage to cartilage and soft tissues.
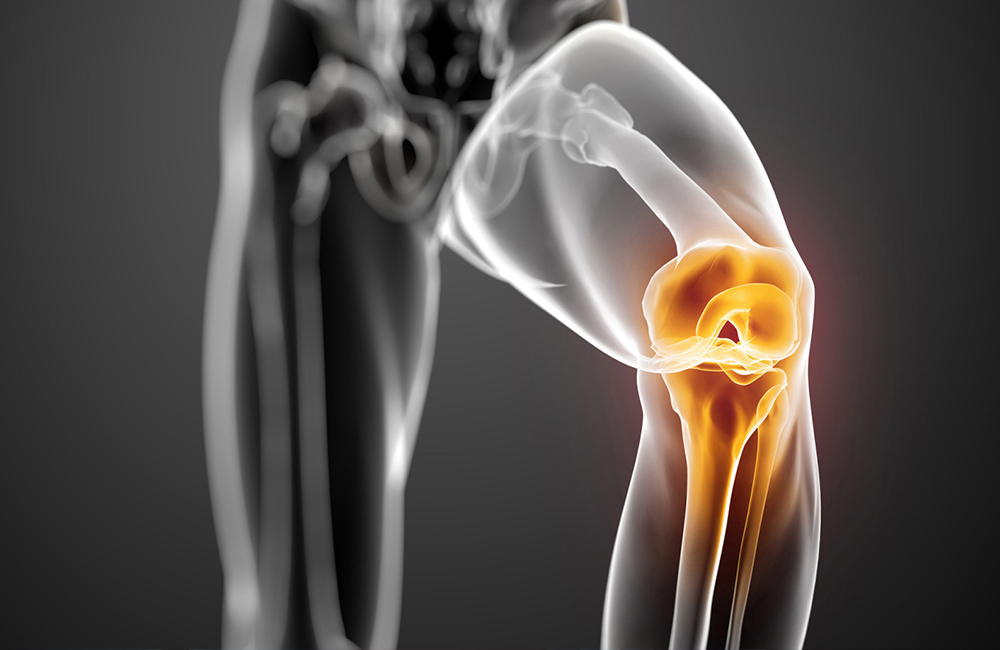
Osteonecrosis or Avascular Necrosis: This occurs when the blood vessels supplying the hip joint are blocked, leading to irreversible damage to the bone in the joint.
Trauma: Following injuries like hip fractures, your doctor may recommend total hip replacement based on your age and overall health.
Tumors in the Hip Joint: Both benign and malignant tumors frequently occur around the hip joint, and total hip replacement surgery may be suggested for their treatment.
Preparation for Total Hip Replacement Surgery
Before surgery, your doctor will examine your hip joint to assess pain, limited mobility, and possible leg length discrepancies. X-rays are usually sufficient for diagnosis, but your doctor may request additional imaging like CT scans or MRIs if necessary.
Some medications may need to be adjusted about one week before surgery. An anesthesiologist will evaluate you 2-3 days prior to determine the most suitable anesthesia method, considering your overall health. Generally, fasting for 6-8 hours before surgery is required.
During Surgery:
Depending on the surgical technique chosen, you will be positioned either on your back or on your side with the hip to be operated on facing up. To reduce the risk of infection, antibiotics will be administered via IV before the surgery. A 15-20 cm incision will be made on the side or front of your hip to expose the hip joint. The damaged femoral head and the acetabulum will be cleaned, and the artificial joint will be implanted. A drain will be placed to prevent fluid accumulation, which will be removed painlessly after 24-48 hours.
The surgery typically lasts 1.5 to 2 hours.
Hip Replacement After a Fracture
After a hip fracture, your doctor may recommend hip replacement surgery based on your overall health and age. Hip fractures are considered semi-emergency situations, and timely surgery is essential for getting the patient back on their feet to avoid complications such as blood clots.
Post-Operative Care for Total Hip Replacement
After the surgery, you will be moved to your room where pain relief medications will be administered via IV. Early mobilization is crucial to prevent blood clots. Many patients start bed exercises on the same day of surgery. The next day, you will be helped to stand and walk.
You will be encouraged to perform breathing exercises and gradually increase your activity level. After being discharged from the hospital, it’s important to continue the prescribed exercises at home.
During the initial 6-12 months of recovery, it is advised to keep a pillow between your legs while sleeping, avoid crossing your legs, and refrain from sitting on low stools.
Outcomes
When performed on the right patient, total hip replacement can yield excellent results, allowing for pain-free and comfortable movement. Most patients can walk independently without aids within 3-4 weeks and return to daily activities. After the first month, your doctor may allow progressively longer walks.
You may be able to drive within 3-4 weeks and return to your daily responsibilities after about a month. Light activities such as walking, swimming, and golf can be resumed after the surgery, while contact sports like football and basketball are generally discouraged.
The goal of hip replacement is to restore your ability to live pain-free and improve your quality of life. A well-executed hip replacement, with appropriate rehabilitation, can have a survival rate of 20-30 years.
Questions and Answers
Are there different types of hip prostheses? Do they all have the same results?
Hip prostheses can be categorized into several groups, including partial hip prosthesis (which replaces only the upper part of the femur) and total hip prosthesis (which replaces both the femoral head and the acetabulum). Total hip prostheses are preferred for active patients who can perform their daily activities independently. Your doctor will provide information about the most suitable prosthesis for you.
Can I have a prosthesis even with significant bone loss?
As we age, osteoporosis can become a significant issue. However, in patients with osteoporosis, certain criteria can be assessed radiologically to determine if cemented prostheses are suitable. Although cemented and uncemented prostheses function similarly, uncemented ones are preferred in patients with good bone quality.
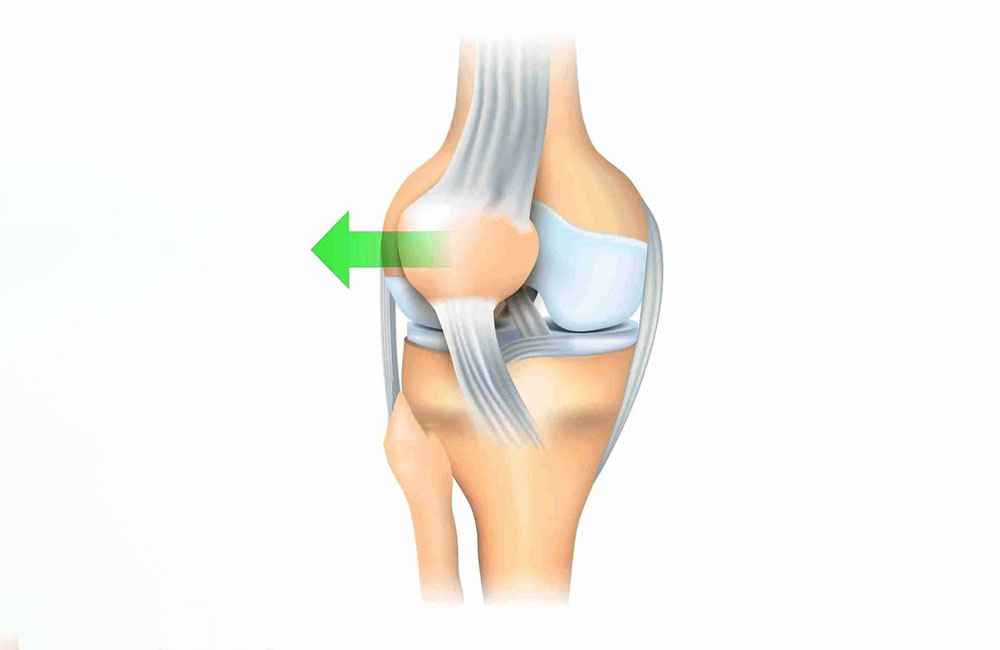
Are there movements I should avoid after hip replacement?
Although the hip prosthesis integrates well with the bone, the wide range of motion of the hip joint can lead to dislocation under certain circumstances. Activities that may cause dislocation include falling, excessive bending, sitting cross-legged, or squatting. Safe ranges of motion will be assessed during surgery, and any necessary restrictions will be discussed with you post-operatively.
I had a prosthesis a long time ago, and it has become loose. Can it be replaced?
Over time, prostheses may wear out or become loose due to factors such as the patient’s age, the properties of the materials used, surgical technique, and the intensity of physical activity post-surgery. In such cases, the loose or damaged parts can be replaced, or in some instances, a complete revision may be necessary, usually with a larger prosthesis.
For detailed information, please visit my YouTube channel: @profdrhalukcabuk